Deep Brain Stimulation (DBS) for Neurological Conditions
Deep brain stimulation (DBS) is an excellent form of technological advancement in health. Over time, the usage of this surgical method to treat neurological conditions such as Parkinson's Disease has become very popular. Researchers suggest that approximately ten million people live with Parkinson's Disease (PD) globally. These neurological conditions are more common in men than in women.
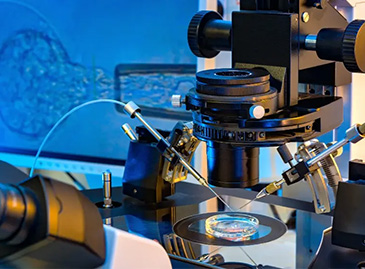
Deep brain stimulation (DBS) involves the insertion of electrodes into some specific part of the brain through a surgical procedure. The significant reason for this insertion is for the electrodes to produce certain electrical impulses. These impulses will help to regulate and block abnormal impulses in the brain.
In addition, the electrode will connect to a pacemaker device ( implantable pulse generator) under the skin of your chest. Wires connecting the electrodes to the pacemaker device will run from under your chest skin to your brain.
Component of deep brain stimulation system (DBS)
DBS consist of four parts, which include;
Pacemaker-like device:
The small device (pulse generator) helps to generate electrical impulses for the electrodes in the brain
Insulated lead wires:
These leads form an attachment at the end of the electrodes implanted in the brain
Extension lead wires:
The extension lead wires help to carry electrical impulses from the pacemaker device under your chest skin to the electrodes in the brain
Handheld programmer:
The device forms the last part of a deep brain stimulation system. It is used for adjusting the signals generated by the pulse generator. It is basically for putting the pulse generator off and on.
In addition, once the system activation is complete, the pacemaker-like device will keep sending electrical pulses to the target site in the brain. The abnormal activity causing symptoms in that part of the brain will get perfect modification and regulation. Experts call this technological procedure the "pacemaker for the brain."
Neurological conditions that can be treated with deep brain stimulation
The technological procedure can help in the treatment of certain neurological conditions such as;
- Epilepsy
- Parkinson's disease
- Essential tumour
- Obsessive-compulsive disorder
- Dystonia
However, researchers indicate that the process of deep brain stimulation for some other conditions is still under review. Some of the requirements for potential DBS treatment include;
- Tourette syndrome
- Cluster headache
- Chronic pain
- Depression
- Multiple sclerosis
- Recovery from stroke
- Huntington's disease
- Alzheimer's disease
- Brain injury
- Anorexia nervosa
However, this treatment is specifically for people with any condition listed above whose symptoms cannot be managed by medications.
Candidate for DBS surgery
Deep brain stimulation is a technology-driven procedure that a team of professional medical practitioners, such as neurosurgeons, performs. However, it would be best to conduct extensive evaluations for candidacy consideration for this surgical procedure. Generally, a medical team consisting of a neurosurgeon, neurologist, neuropsychologist, and psychiatrist will help carry out the extensive evaluation.
Furthermore, if medications are enough to manage your condition, you will not require deep brain stimulation. However, the right candidate for DBS will meet the following criteria;
- Symptoms are not improving despite the usage of medications
- The symptoms are affecting the quality of your life
- Your body does not tolerate the medicines given by your doctor.
Benefits of deep brain stimulation
The following are the advantages of DBS;
- It does not cause permanent brain damage
- The stimulation is reversible and adjustable
- DBS offers room for turning the stimulator off if you can not tolerate the side effects.
Risks
Experts suggest that DBS comes with low risk. But, like other surgical procedures, it has some complications, too. Stimulating the brain has some side effects and dangers, too. Generally, the risk can either be from or after the surgery.
Risks from the surgical procedure
Surgeries involve making small or large incisions, depending on the type of surgery. Your neurosurgeon will make small holes in your skull to implant the electrodes for DBS. However, this may come with some risks, which include;
- Infection
- Possible heart complications
- Breathing problem
- Seizure
- Lead misplacement
- Bleeding in the brain
Side effects after the surgery
Furthermore, the possible side effects that may occur after this procedure include;
- Hardware complications
- Headache
- Stroke
- Pain in the implantation site
However, your doctor will turn the system on a few weeks from the surgery date after the procedure. In addition, your neurosurgeon will help you adjust the system to the best settings. However, some reports show that deep brain stimulation can affect swimming. But you can speak with your doctor if you love swimming. They will inform you of the possible water safety precautions you should observe.
The possible effect of stimulation
Stimulating the brain has some side effects. Although, this can be managed effectively by your health team. However, let's take a look at the most familiar effects, which include;
- Face or arm muscle tightness
- Vision problems
- Frequent mood swing
- Balancing and speech problems.
In addition, for proper preparation, you must consider the risks and the benefits of deep brain stimulation (DBS). If you have a history of any medical condition, inform your doctor. They will help you make an informed decision before DBS surgery.
Procedures for deep brain stimulation
A neurosurgeon will carry out this procedure with the help of other medical professionals. Before the commencement of the surgical procedure, your surgeon will place a head frame on your head. The head frame (stereotactic head frame) keeps your head from moving during brain imaging. The deep brain stimulation procedure is in two stages.
Firstly, you will undergo computed tomography (CT) or magnetic resonance imaging (MRI) scans before the procedure. These scans are for your surgeon to know the target area and electrode placement guidance. Furthermore, a small hole will be made in your skull. The neurosurgeon will implant electrodes with leads into the site of the symptoms in your brain through these tiny holes.
Secondly, your surgeon will implant the pulse-generating device under the skin of your chest. A wire extension will be attached to the lead at the end of the electrodes existing in the brain. Subsequently, the neurosurgeon will pass these wires under the skin behind your ear to the pulse-generating machine in the chest skin. Your surgeon will program this pulse generator to send continuous electrical pulses to your brain.
Finally, a few weeks after the implantation, your neurosurgeon will help turn the pulse generator on with a handheld device. However, an adjustment will be made to this pulse generated until there is an improvement in the symptoms. Adjusting the pulse generator to reach the optimal setting may take a few months. Frequently, stimulating the brain is constant. But, your surgeon may advise you to put it off at night and on it back during the day.
Possible Result
Remembering that deep brain stimulation cannot work for everyone would be best. DBS will not cure your disease. But, it can improve the quality of your life by reducing the symptoms of neurological conditions. In rare cases, your doctor might still prescribe some medications. But, there is an assurance that if this procedure works for you, you will live a better life afterwards. Please always discuss this with your doctor; they will help you make an informed decision without stress.
How do you live with the stimulator?
Once your surgeon has programmed your stimulator, you will be discharged to leave for your house. Before going, your surgeon will educate you on adjusting this stimulator with the handheld controller. With the controller, you can increase the strength of the stimulator or turn it on and off. You need a charging unit if your stimulator comes with a rechargeable battery. You can charge it for approximately one to two hours per week. Your surgeon will inform you of the choice of primary or rechargeable cells before the surgery.
Bunion Surgery Price Turkey